WHAT IS DIABETES?
The body’s main source of energy is glucose. Glucose is a sugar that the body derives from carbohydrates found in the food. Blood glucose is the amount of sugar that is in the blood, for the body to use as energy (1,2).
After a meal, the levels of blood glucose in the body increases. This increase triggers the pancreas to release a hormone known as insulin into the bloodstream. Insulin handles the transportation of sugars (from ingested food or beverages) to the cells of the body. The cells then convert the sugars into energy for the body to use (2,3).
Additionally, insulin handles the storage of sugar by the liver and muscles. Insulin also ensures that new sugar is not made in the liver, causing a reduction in the blood sugar levels. The opposite mechanism occurs when the blood sugar levels are low. The pancreas releases a hormone known as glucagon. Glucagon makes the liver release its stored sugar and allows the liver to make new sugars for use as energy. An increase in blood sugar levels stops the release of glucagon (3).
What System Causes Diabetes?
Diabetes is a metabolic disease. It develops when the blood glucose or blood sugar levels become too high. This occurs due to a lack of insulin production or when the body is not using the produced insulin as it should. Such occurrences cause the glucose to remain in the blood; instead of going to the cells. There are two main types of diabetes: Type 1 diabetes and Type 2 diabetes (3,4).
What Body Systems are Affected by Diabetes?
One of the reasons that diabetes can be such a difficult and devastating disease is due to the fact that all body systems are affected. If your cells cannot absorb sugar and your blood sugar is too high, it affects your circulatory, cardiovascular, musculoskeletal, endocrinal, digestive, and nervous systems(150).
How Does Diabetes Affect the Nervous System?
Peripheral neuropathy, nerve damage primarily of the legs, feet, toes, arms, hands, and fingers is one of the most common complications of diabetes. If not kept in check, it can lead to amputation.
About 30 percent of people with diabetes have autonomic neuropathy which affects involuntary functions like digestion(150).
How Does Diabetes Affect the Digestive System?
As discussed, nerve damage to the digestive system can occur. Gastroparesis is a condition that may occur, which keeps food from moving from the stomach into the small intestine(150), by disrupting the stomach’s contractions(151).
Diabetes is a metabolic disease. It develops when the blood glucose or blood sugar levels become too high. This occurs due to a lack of insulin production or when the body is not using the produced insulin as it should. Such occurrences cause the glucose to remain in the blood; instead of going to the cells. There are two main types of diabetes: Type 1 diabetes and Type 2 diabetes (3,4).
Type 1 Diabetes
Type 1 diabetes occurs when the body’s immune system attacks the beta cells of the pancreas. These cells are responsible for producing insulin. When this occurs, these cells do not produce sufficient insulin or even any insulin at all. Type 1 diabetes is most common in children and adolescents. This type of diabetes has been formerly known as insulin-dependent diabetes or juvenile onset diabetes. Persons with Type 1 diabetes require constant insulin replacement therapy (4,5,6,7).
Type 2 Diabetes
Type 2 Diabetes occurs when the body is resistant to the effects of insulin. There are two main distinctions between Type 1 and Type 2 diabetes. Persons with type 2 diabetes are not dependent on insulin, as the pancreas still secretes insulin. Additionally, there is no autoimmune destruction of the pancreas. Type 2 diabetes is more common than type 1 diabetes, accounting for over 90% of all diabetes diagnoses. Type 2 diabetes is typically seen in middle-aged to older adults and is usually a result of obesity (4,5,6,8).
RISK FACTORS AND SYMPTOMS OF DIABETES
Type 1 Diabetes
Symptoms for Type 1 Diabetes include (9,10,11):
- Abnormally extreme and excessive thirst
- Abnormal and excessive production of urine
- Frequently waking up at night to urinate
- Urinary incontinence
- Fatigue
- Unexplained weight loss
- Lack of appetite
- Vomiting
- Constipation
- Stomach pains
- Blurry vision
Risk factors for Type 1 diabetes include:
- Genetics and family history of diabetes (12,13)
- Lack of vitamin D in mother’s during pregnancy (14)
- Increased intake of cow’s milk during infancy and childhood (15,16)
- Early (less than 4 months old) and late (more than 6 months old) exposure to solid food for infants (17)
- Dietary gluten in childhood (18,19)
- Prenatal factors (20,21,22)
Type 2 Diabetes
Symptoms for Type 2 diabetes include (23,24):
- Fatigue
- Weight loss
- Excessive abnormal thirst
- Frequent urination
- Infections in the genital areas, urinary tract, mouth, and skin
- Mood changes and feelings of confusion
- Excessive itching
- Dry mouth
- Inflammation of mouth and lips
- Impaired vision
- Numbness in feet
- Erectile dysfunction
- Patches of darkened skin in armpits and neck
Risk factors for Type 2 diabetes include (23,25):
- Genetics and family history of diabetes (26)
- Age – type 2 diabetes is usually seen in adults over the age of 40 years
- Obesity and large waist circumference
- High blood pressure
- Lack of physical activity
- Smoking (27,28,29)
- Diets high in sugars, fried foods, red meats, and carbohydrates (29,30)
- Vitamin D and K deficiency (31,32,33,34,35)
SILENT HEART ATTACKS
4 SIGNS OF A SILENT HEART ATTACK
Silent ischemia [lack of oxygen] or a silent heart attack can go by unnoticed or ignored, but still does damage and has significant effects. The 4 persistent signs that may indicate you have suffered a silent heart attack are:
- Chronic fatigue
- Persistent indigestion
- Flu-like symptoms
- Muscle pain mistaken for a strain or pull(152)
WHAT CAUSES A SILENT HEART ATTACK?
As with any heart attack, a silent heart attack is caused by a buildup of plaque that causes a reduction of blood flow to the heart. This buildup of plaque can be produced by:
- Smoking
- High blood pressure
- High cholesterol
- Family history
- Obesity(152)
WHAT DOES A SILENT HEART ATTACK FEEL LIKE?
The symptoms are the same as a full-fledged heart attack, just usually not as severe or as prolonged. Even these mild symptoms should be taken seriously:
- Chest pressure
- Pain in the chest, jaw, shoulder, back, and arm
- Numbness
- Shortness of breath(153)
CAN A HEART ATTACK RAISE BLOOD SUGAR?
Hyperglycemia, or high blood sugar, is a response of the body against trauma or stress, both physical and psychological. Trauma triggers the body’s stress responses like hormones and creates changes in how carbohydrates, proteins, and fats are metabolized(154).
DIABETES FACTS AND STATISTICS
Reports for 2017 show that 9.4 % of the US population, which is 30.3 million persons, have diabetes (36). Type 1 diabetes is less common than Type 2 diabetes, with only about 5% of all diabetes cases being Type 1 (37).
Is There a Diabetes Epidemic?
Technically, diabetes is not and cannot be an epidemic, because it is not an infectious disease, but it is approaching epidemic proportions. As global rates of obesity increase, so does the occurrence of diabetes. Diabetes.co.uk is a global diabetes community, and it estimates that 1 in 11 people, 415 million globally, have diabetes, and if things do not change, that number could increase to 642 million by the year 2040(155).
MEDICAL TREATMENT OF DIABETES
Type 1 Diabetes
The mainstay treatment for Type 1 diabetes is insulin replacement therapy, as the body is producing little to no insulin at all. A drug known as Pramlintide, is also used in addition to insulin therapy. It mimics the actions of the enzyme Amylin, which is no longer produced by the body if a person has Type 1 diabetes (38).
Pramlintide works to improve glycemic control, reduce glucose levels and body weight in persons also taking insulin after meals (39). Pramlintide is an intravenous drug. Brand names include at Symlin or SymlinPen. Side effects of Pramlintide include dizziness, fainting, seizures, nausea, vomiting, stomach pains, rapid heartbeat, profuse sweating, and irritation at injection site (40).
Type 2 Diabetes
Biguanides (Metformin) works by increasing insulin sensitivity, decreasing absorption of glucose from the gastrointestinal tract, improving glucose uptake and inhibiting liver production of glucose (26). Marketed as Glucophage, Glumteza, DM2, Fortamet, Riomet (41,42). Side effects include fever, chills, feeling of confusion, rapid heartbeat, nausea, vomiting, stomach pain, muscle pain or cramps, fatigue, diarrhea, metallic taste in mouth (42).
Sulfonylureas (Glyburide & Glipizide) works by stimulating insulin secretion from beta cells in the pancreas. Glyburide is long-acting and can cause hypoglycemia. It is not recommended for use with elderly patients (26). Marketed as Diabeta, Micronase, Glynase, Glucotrol, and Amaryl (41). Side effects include weight gain, nausea, skin irritation, jaundice, hepatitis, Growth Hormone disorder, cardiac problems, erectile dysfunction, and malignancy (43,44).
Meglitinides (Repaglinide and Nateglinide) work by stimulating insulin secretion from beta cells in the pancreas. These drugs have a rapid onset and are short-acting (26). Marketed as Pradin and Starlix (41). Side effects include skin rash and blisters, difficulty breathing, seizures, trembling, rapid heart rate, feelings of confusion, weight gain, runny nose, coughing, and sore throat (45).
Thiazolidinediones (Pioglitazone) works by decreasing resistance to insulin. Marketed as Actos and Avandia (41). Side effects include edema, heart failure, weight gain, bone loss (risk of fractures in women) (46,47).
Alpha-Glucosidase Inhibitors (Acarbose, Voglibose, and Miglitol) works by delaying the absorption of glucose. Marketed as Precose and Glyset (41). Side effects include diarrhea and flatulence (48).
Dipeptidyl-Peptidase IV Inhibitors (Sitagliptin and Saxagliptin) are taken together with metformin, thiazolidinediones, and insulin (26). Marketed as Januvia and Janumet (41).
Side effects include upper respiratory tract infections, swelling of nasal passages and back of the throat, headache, anaphylaxis, angioedema, Stevens-Johnson syndrome (severe skin disorder), pancreatitis, hypoglycemia when used with sulfonylurea (49,50).
CONVENTIONAL TREATMENT OF DIABETES AND PRACTICES TO SUPPORT HEALTHY BLOOD SUGAR LEVELS
Practices to Support Healthy Blood Sugar Levels:
For Type 2 Diabetes, research has shown that a healthy diet and exercise can support healthy glucose levels. This aids in the prevention of developing diabetes. Lifestyle modifications such as healthy weight loss and increase physical activity can contribute to the prevention of diabetes and to supporting the management of persons living with diabetes (51,52,53,54).
Effective Home Remedies for Diabetes
Again, diet and exercise are key when it comes to controlling diabetes. Follow a diet rich in low-sugar fruits (you may have to avoid high-sugar fruits like pineapple and mango) as well as vegetables, whole grains, and lean meats. Stay away from refined sugar and simple carbohydrates. A low glycemic-index diet is a good framework(156).
Dehydration can raise blood sugar levels, so make sure you drink plenty of water. Also, try to reduce stress and get plenty of good restorative sleep(156).
Natural Supplements That Support Healthy Blood Sugar Levels:
- Chromium (55,56,57)
- Cinnamon Extract (58,59,60,61)
- Gymnema (62,63,64,65)
- Alpha Lipoic Acid (66,67,68,69,83,84,85,86)
- Bilberry (70,71)
- Fenugreek Seed (72,73,74)
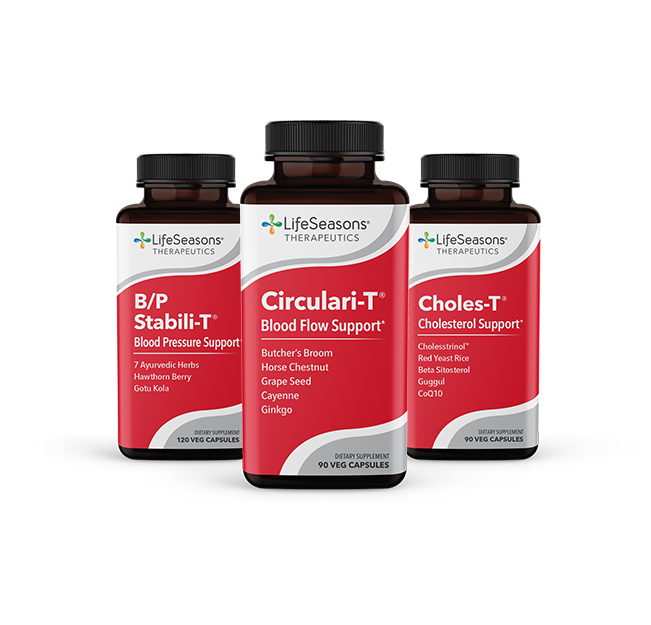
- Butcher’s Broom (75)
- Bitter melon (76,77,78)
- Banaba (79,87,88)
- Holy Basil (80)
- Vanadium (81,82,89,90,91,92,93)
- Aloe Vera (94,95,96,97,98,99,100)
- American ginseng (101,102,103)
- Barberine (104,105,106,107)
- Black seed (108,109,110)
- Blond psyllium (111,112,113,114,115,116,117,118)
- Caffeine (119,120,121,122,123,124)
- Flaxseed (125,126,127,128,129)
- Glucomannan (130,131,132,133,134,135)
- Magnesium (136,137,138,139,140,141)
- Gotu kola (142,143)
- Bitter melon (144,145,146,147,148,149)
REFERENCES
- Glucose – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022906/. Accessed May 15, 2018.
- What is Diabetes? | NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. 2018. Available at: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes. Accessed May 15, 2018.
- Blood Glucose – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024697/. Accessed May 15, 2018.
- American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2009;33(Supplement_1): S62-S69. doi:10.2337/dc10-s062.
- Kharroubi A, Darwish H. Diabetes mellitus: The epidemic of the century. World J Diabetes. 2015;6(6):850-867. doi:10.4239/wjd. v6.i6.850.
- Dean L, McEntyre J. Introduction to Diabetes. Ncbinlmnihgov. 2018. Available at: https://www.ncbi.nlm.nih.gov/books/NBK1671/. Accessed May 15, 2018.
- Type 1 Diabetes – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024702/. Accessed May 15, 2018.
- Type 2 Diabetes – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0024703/. Accessed May 15, 2018.
- Jasiński D, Pilecki O, Robak-Kontna K, Zbikowska-Bojko M. Analysis of type 1 diabetes mellitus symptoms at admission to hospital. Endokrynol Diabetol Chor Przemiany Materii Wieku Rozw. 2003;9(2):83-87. Available at: https://www.ncbi.nlm.nih.gov/pubmed/14575617. Accessed May 15, 2018.
- Usher-Smith J, Thompson M, Zhu H, Sharp S, Walter F. The pathway to diagnosis of type 1 diabetes in children: a questionnaire study. BMJ Open. 2015;5(3):e006470-e006470. doi:10.1136/bmjopen-2014-006470.
- Type 1 Diabetes | NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. 2018. Available at: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-1-diabetes. Accessed May 15, 2018.
- Wu Y, Ding Y, Gao J, Tanaka Y, Zhang W. Risk Factors and Primary Prevention Trials for Type 1 Diabetes. Int J Biol Sci. 2013;9(7):666-679. doi:10.7150/ijbs.6610.
- Pociot F, Lernmark Å. Genetic risk factors for type 1 diabetes. The Lancet. 2016;387(10035):2331-2339. doi:10.1016/s0140-6736(16)30582-7.
- Sorensen I, Joner G, Jenum P, Eskild A, Torjesen P, Stene L. Maternal Serum Levels of 25-Hydroxy-Vitamin D During Pregnancy and Risk of Type 1 Diabetes in the Offspring. Diabetes. 2011;61(1):175-178. doi:10.2337/db11-0875.
- Virtanen S, Laara E, Hypponen E et al. Cow’s milk consumption, HLA-DQB1 genotype, and type 1 diabetes: a nested case-control study of siblings of children with diabetes. Childhood diabetes in Finland study group. Diabetes. 2000;49(6):912-917. doi:10.2337/diabetes.49.6.912.
- Lamb M, Miller M, Seifert J et al. The effect of childhood cow’s milk intake and HLA-DR genotype on risk of islet autoimmunity and type 1 diabetes: The Diabetes Autoimmunity Study in the Young. Pediatr Diabetes. 2014;16(1):31-38. doi:10.1111/pedi.12115.
- Frederiksen B, Kroehl M, Lamb M et al. Infant Exposures and Development of Type 1 Diabetes Mellitus. JAMA Pediatr. 2013;167(9):808. doi:10.1001/jamapediatrics.2013.317.
- Antvorskov J, Josefsen K, Engkilde K, Funda D, Buschard K. Dietary gluten and the development of type 1 diabetes. Diabetologia. 2014;57(9):1770-1780. doi:10.1007/s00125-014-3265-1.
- Hogg-Kollars S, Al Dulaimi D, Tait K, Rostami K. Type 1 diabetes mellitus and gluten induced disorders. Gastroenterol Hepatol Bed Bench. 2014;7(4):189-197. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4185872/. Accessed May 16, 2018.
- Samad Majeed A, Hassan M. Risk Factors for Type 1 Diabetes Mellitus among Children and Adolescents in Basrah. Oman Med J. 2011;26(3):189-195. doi:10.5001/omj.2011.46.
- Copenhaver M, Hoffman R. Type 1 diabetes: where are we in 2017. Transl Pediatr. 2017;6(4):359-364. doi:10.21037/tp.2017.09.09.
- Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. The Lancet. 2016;387(10035):2340-2348. doi:10.1016/s0140-6736(16)30507-4.
- Ramachandran A. Know the signs and symptoms of diabetes. Indian Journal of Medical Research. 2014;140(5):579-581.
- Drivsholm T, de Fine Olivarius N, Nielsen A, Siersma V. Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycaemia, blood pressure and weight. Diabetologia. 2005;48(2):210-214. doi:10.1007/s00125-004-1625-y.
- Wu Y, Ding Y, Tanaka Y, Zhang W. Risk Factors Contributing to Type 2 Diabetes and Recent Advances in the Treatment and Prevention. Int J Med Sci. 2014;11(11):1185-1200. doi:10.7150/ijms.10001.
- Olokoba A, Obateru O, Olokoba L. Type 2 Diabetes Mellitus: A Review of Current Trends. Oman Med J. 2012;27(4):269-273. doi:10.5001/omj.2012.68.
- Willi C, Bodenmann P, Ghali W, Faris P, Cornuz J. Active Smoking and the Risk of Type 2 Diabetes. JAMA. 2007;298(22):2654. doi:10.1001/jama.298.22.2654.
- Chang S. Smoking and Type 2 Diabetes Mellitus. Diabetes Metab J. 2012;36(6):399. doi:10.4093/dmj.2012.36.6.399.
- Maddatu J, Anderson-Baucum E, Evans-Molina C. Smoking and the risk of type 2 diabetes. Translational Research. 2017;184:101-107. doi:10.1016/j.trsl.2017.02.004.
- Hu F, Liu S, van Dam R. Diet and risk of Type II diabetes: the role of types of fat and carbohydrate. Diabetologia. 2001;44(7):805-817. doi:10.1007/s001250100547.
- Sami W, Ansari T, Shafique Butt N, Rashid Ab Hamid M. Effect of diet on type 2 diabetes mellitus: A review. Int J Health Sci (Qassim). 2017;11(2):65-71. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5426415/. Accessed May 17, 2018.
- Pittas A, Sun Q, Manson J, Dawson-Hughes B, Hu F. Plasma 25-Hydroxyvitamin D Concentration and Risk of Incident Type 2 Diabetes in Women. Diabetes Care. 2010;33(9):2021-2023. doi:10.2337/dc10-0790.
- Mitri J, Dawson-Hughes B, Hu F, Pittas A. Effects of vitamin D and calcium supplementation on pancreatic β cell function, insulin sensitivity, and glycemia in adults at high risk of diabetes: the Calcium and Vitamin D for Diabetes Mellitus (CaDDM) randomized controlled trial. Am J Clin Nutr. 2011;94(2):486-494. doi:10.3945/ajcn.111.011684.
- Takiishi T, Gysemans C, Bouillon R, Mathieu C. Vitamin D and Diabetes. Endocrinol Metab Clin North Am. 2010;39(2):419-446. doi:10.1016/j.ecl.2010.02.013.
- Wolden-Kirk H, Overbergh L, Christesen H, Brusgaard K, Mathieu C. Vitamin D and diabetes: Its importance for beta cell and immune function. Mol Cell Endocrinol. 2011;347(1-2):106-120. doi:10.1016/j.mce.2011.08.016.
- National Diabetes Statistics Report | Data & Statistics | Diabetes | CDC. Cdcgov. 2018. Available at: https://www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed May 17, 2018.
- Type 1 Diabetes | Basics | Diabetes | CDC. Cdcgov. 2018. Available at: https://www.cdc.gov/diabetes/basics/type1.html. Accessed May 17, 2018.
- Chamberlain J, Kalyani R, Leal S et al. Treatment of Type 1 Diabetes: Synopsis of the 2017 American Diabetes Association Standards of Medical Care in Diabetes. Ann Intern Med. 2017;167(7):493. doi:10.7326/m17-1259.
- Edelman S, Maier H, Wilhelm K. Pramlintide in the Treatment of Diabetes Mellitus. BioDrugs. 2008;22(6):375-386. doi:10.2165/0063030-200822060-00004.
- Pramlintide (By injection) – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0011808/?report=details. Accessed May 17, 2018.
- Nyenwe E, Jerkins T, Umpierrez G, Kitabchi A. Management of type 2 diabetes: evolving strategies for the treatment of patients with type 2 diabetes. Metabolism. 2011;60(1):1-23. doi:10.1016/j.metabol.2010.09.010.
- Metformin (By mouth) – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0011121/?report=details. Accessed May 17, 2018.
- Sola D, Rossi L, Schianca G et al. State of the art paper Sulfonylureas and their use in clinical practice. Archives of Medical Science. 2015;4:840-848. doi:10.5114/aoms.2015.53304.
- Sehra D, Sehra S, Sehra S. Sulfonylureas: do we need to introspect safety again?. Expert Opin Drug Saf. 2011;10(6):851-861. doi:10.1517/14740338.2011.583234.
- Repaglinide (By mouth) – National Library of Medicine – PubMed Health. PubMed Health. 2018. Available at: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0011962/?report=details. Accessed May 17, 2018.
- Rizos C, Elisaf M, Mikhailidis D, Liberopoulos E. How safe is the use of thiazolidinediones in clinical practice?. Expert Opin Drug Saf. 2008;8(1):15-32. doi:10.1517/14740330802597821.
- Shah P, Mudaliar S. Pioglitazone: side effect and safety profile. Expert Opin Drug Saf. 2010;9(2):347-354. doi:10.1517/14740331003623218.
- Derosa G, Maffioli P. Mini-Special Issue paper Management of diabetic patients with hypoglycemic agents α-Glucosidase inhibitors and their use in clinical practice. Archives of Medical Science. 2012;5:899-906. doi:10.5114/aoms.2012.31621.
- White J. Dipeptidyl Peptidase-IV Inhibitors: Pharmacological Profile and Clinical Use. Clinical Diabetes. 2008;26(2):53-57. doi:10.2337/diaclin.26.2.53.
- Pathak R, Barna Bridgeman M. Dipeptidyl Peptidase-4 (DPP-4) Inhibitors In the Management of Diabetes. Pharmacy and Therapeutics. 2010;35(9):509-513. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2957740/. Accessed May 17, 2018.
- Look AHEAD Research Group. Reduction in Weight and Cardiovascular Disease Risk Factors in Individuals With Type 2 Diabetes: One-Year Results of the Look AHEAD Trial. Diabetes care. 2007;30(6):1374-1383. doi:10.2337/dc07-0048.
- Stern L, Iqbal N, Seshadri P et al. The Effects of Low-Carbohydrate versus Conventional Weight Loss Diets in Severely Obese Adults: One-Year Follow-up of a Randomized Trial. Ann Intern Med. 2004;140(10):778. doi:10.7326/0003-4819-140-10-200405180-00007.
- Pan X, Li G, Hu Y et al. Effects of Diet and Exercise in Preventing NIDDM in People With Impaired Glucose Tolerance: The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537-544. doi:10.2337/diacare.20.4.537.
- Goldhaber-Fiebert J, Goldhaber-Fiebert S, Tristan M, Nathan D. Randomized Controlled Community-Based Nutrition and Exercise Intervention Improves Glycemia and Cardiovascular Risk Factors in Type 2 Diabetic Patients in Rural Costa Rica. Diabetes Care. 2003;26(1):24-29. doi:10.2337/diacare.26.1.24.
- Anderson R. Chromium, Glucose Intolerance and Diabetes. J Am Coll Nutr. 1998;17(6):548-555. doi:10.1080/07315724.1998.10718802.
- Yin R, Phung O. Effect of chromium supplementation on glycated hemoglobin and fasting plasma glucose in patients with diabetes mellitus. Nutr J. 2015;14(1). doi:10.1186/1475-2891-14-14.
- Rabinovitz H, Friedensohn A, Leibovitz A, Gabay G, Rocas C, Habot B. Effect of Chromium Supplementation on Blood Glucose and Lipid Levels in Type 2 Diabetes Mellitus Elderly Patients. International Journal for Vitamin and Nutrition Research. 2004;74(3):178-182. doi:10.1024/0300-9831.74.3.178.
- Anderson R, Zhan Z, Luo R et al. Cinnamon extract lowers glucose, insulin and cholesterol in people with elevated serum glucose. J Tradit Complement Med. 2016;6(4):332-336. doi:10.1016/j.jtcme.2015.03.005.
- Allen R, Schwartzman E, Baker W, Coleman C, Phung O. Cinnamon Use in Type 2 Diabetes: An Updated Systematic Review and Meta-Analysis. The Annals of Family Medicine. 2013;11(5):452-459. doi:10.1370/afm.1517.
- Qin B, Panickar K, Anderson R. Cinnamon: Potential Role in the Prevention of Insulin Resistance, Metabolic Syndrome, and Type 2 Diabetes. J Diabetes Sci Technol. 2010;4(3):685-693. doi:10.1177/193229681000400324.
- Mang B, Wolters M, Schmitt B et al. Effects of a cinnamon extract on plasma glucose, HbA1c, and serum lipids in diabetes mellitus type 2. Eur J Clin Invest. 2006;36(5):340-344. doi:10.1111/j.1365-2362.2006.01629.x.
- Tiwari P, Mishra B, Sangwan N. Phytochemical and Pharmacological Properties of Gymnema sylvestre: An Important Medicinal Plant. Biomed Res Int. 2014;2014:1-18. doi:10.1155/2014/830285.
- Tiwari P, Ahmad K, Hassan Baig M. Gymnema sylvestre for Diabetes: From Traditional Herb to Future’s Therapeutic. Curr Pharm Des. 2017;23(11):1667-1676. doi:10.2174/1381612823666161108162048.
- Pothuraju R, Sharma R, Chagalamarri J, Jangra S, Kumar Kavadi P. A systematic review ofGymnema sylvestrein obesity and diabetes management. J Sci Food Agric. 2013;94(5):834-840. doi:10.1002/jsfa.6458.
- Baskaran K, Ahamath B, Shanmugasundaram K, Shanmugasundaram E. Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol. 1990;30(3):295-305. doi:10.1016/0378-8741(90)90108-6.
- Golbidi S, Badran M, Laher I. Diabetes and Alpha Lipoic Acid. Front Pharmacol. 2011;2(69). doi:10.3389/fphar.2011.00069.
- Ibrahimpasic K. Alpha Lipoic Acid and Glycaemic Control in Diabetic Neuropathies at Type 2 Diabetes Treatment. Medical Archives. 2013;67(1):7. doi:10.5455/medarh.2013.67.7-9.
- Rochette L, Ghibu S, Muresan A, Vergely C. Alpha-lipoic acid: molecular mechanisms and therapeutic potential in diabetes. Can J Physiol Pharmacol. 2015;93(12):1021-1027. doi:10.1139/cjpp-2014-0353.
- Papanas N, Ziegler D. Efficacy of α-lipoic acid in diabetic neuropathy. Expert Opin Pharmacother. 2014;15(18):2721-2731. doi:10.1517/14656566.2014.972935.
- Asgary S, RafieianKopaei M, Sahebkar A, Shamsi F, Goli-malekabadi N. Anti-hyperglycemic and anti-hyperlipidemic effects ofVaccinium myrtillusfruit in experimentally induced diabetes (antidiabetic effect ofVaccinium myrtillusfruit). J Sci Food Agric. 2015;96(3):764-768. doi:10.1002/jsfa.7144.
- Hoggard N, Cruickshank M, Moar K et al. A single supplement of a standardised bilberry (Vaccinium myrtillus L.) extract (36 % wet weight anthocyanins) modifies glycaemic response in individuals with type 2 diabetes controlled by diet and lifestyle. J Nutr Sci. 2013;2. doi:10.1017/jns.2013.16.
- Gaddam A, Galla C, Thummisetti S, Marikanty R, Palanisamy U, Rao P. Role of Fenugreek in the prevention of type 2 diabetes mellitus in prediabetes. Journal of Diabetes & Metabolic Disorders. 2015;14(1). doi:10.1186/s40200-015-0208-4.
- Sharma R, Raghuram T, Rao N. Effect of fenugreek seeds on blood glucose and serum lipids in type I diabetes. Eur J Clin Nutr. 1990;44(4):301-306.
- Kassaian N, Azadbakht L, Forghani B, Amini M. Effect of Fenugreek Seeds on Blood Glucose and Lipid Profiles in Type 2 Diabetic Patients. International Journal for Vitamin and Nutrition Research. 2009;79(1):34-39. doi:10.1024/0300-9831.79.1.34.
- Redman D. Ruscus aculeatus(Butcher’s Broom) as a Potential Treatment for Orthostatic Hypotension, with a Case Report. The Journal of Alternative and Complementary Medicine. 2000;6(6):539-549. doi:10.1089/acm.2000.6.539.
- Joseph B, Jini D. Antidiabetic effects of Momordica charantia (bitter melon) and its medicinal potency. Asian Pac J Trop Dis. 2013;3(2):93-102. doi:10.1016/s2222-1808(13)60052-3.
- Alam M, Uddin R, Subhan N, Rahman M, Jain P, Reza H. Beneficial Role of Bitter Melon Supplementation in Obesity and Related Complications in Metabolic Syndrome. J Lipids. 2015;2015:1-18. doi:10.1155/2015/496169.
- Krawinkel M, Keding G. Bitter Gourd (Momordica charantia):A Dietary Approach to Hyperglycemia. Nutr Rev. 2006;64(7):331-337. doi:10.1111/j.1753-4887.2006.tb00217.x.
- Stohs S, Miller H, Kaats G. A Review of the Efficacy and Safety of Banaba (Lagerstroemia speciosa L.) and Corosolic Acid. Phytotherapy Research. 2011:n/a-n/a. doi:10.1002/ptr.3664.
- Agrawal P, Rai V, Singh R. Randomized placebo-controlled, single blind trial of holy basil leaves in patients with noninsulin-dependent diabetes mellitus. Int J Clin Pharmacol Ther. 1996;34(9):406-409.
- Poucheret P, Verma S, Grynpas M, McNeill J. Vanadium and diabetes. Mol Cell Biochem. 1998;188(1-2):73-80.
- Thompson K, Lichter J, LeBel C, Scaife M, McNeill J, Orvig C. Vanadium treatment of type 2 diabetes: A view to the future. J Inorg Biochem. 2009;103(4):554-558. doi:10.1016/j.jinorgbio.2008.12.003.
- Konrad T, Vicini P, Kusterer K et al. alpha-Lipoic acid treatment decreases serum lactate and pyruvate concentrations and improves glucose effectiveness in lean and obese patients with type 2 diabetes. Diabetes Care. 1999;22(2):280-287. doi:10.2337/diacare.22.2.280.
- Jacob S, Henriksen E, Tritschler H, Augustin H, Dietze G. Improvement of insulin-stimulated glucose-disposal in type 2 diabetes after repeated parenteral administration of thioctic acid. Experimental and Clinical Endocrinology & Diabetes. 2009;104(03):284-288. doi:10.1055/s-0029-1211455.
- Jacob S, Henriksen E, Schiemann A et al. Enhancement of glucose disposal in patients with type 2 diabetes by alpha-lipoic acid. Arzneimittelforschung. 1995;45(8):872-874. Available at: https://www.ncbi.nlm.nih.gov/pubmed/7575750. Accessed May 22, 2018.
- Jacob S, Ruus P, Hermann R et al. Oral administration of rac-α-lipoic acid modulates insulin sensitivity in patients with type-2 diabetes mellitus: a placebo-controlled pilot trial. Free Radical Biology and Medicine. 1999;27(3-4):309-314. doi:10.1016/s0891-5849(99)00089-1.
- Judy W, Hari S, Stogsdill W, Judy J, Naguib Y, Passwater R. Antidiabetic activity of a standardized extract (Glucosol™) from Lagerstroemia speciosa leaves in Type II diabetics. J Ethnopharmacol. 2003;87(1):115-117. doi:10.1016/s0378-8741(03)00122-3.
- Tjokroprawiro A, Murtiwi S, Tjandrawinata R. DLBS3233, a combined bioactive fraction of Cinnamomum burmanii and Lagerstroemia speciosa, in type-2 diabetes mellitus patients inadequately controlled by metformin and other oral antidiabetic agents. Journal of Complementary and Integrative Medicine. 2016;13(4). doi:10.1515/jcim-2016-0031.
- Halberstam M, Cohen N, Shlimovich P, Rossetti L, Shamoon H. Oral vanadyl sulfate improves insulin sensitivity in NIDDM but not in obese nondiabetic subjects. Diabetes. 1996;45(5):659-666. doi:10.2337/diabetes.45.5.659.
- Cohen N, Halberstam M, Shlimovich P, Chang C, Shamoon H, Rossetti L. Oral vanadyl sulfate improves hepatic and peripheral insulin sensitivity in patients with non-insulin-dependent diabetes mellitus. Journal of Clinical Investigation. 1995;95(6):2501-2509. doi:10.1172/jci117951.
- Boden G, Chen X, Ruiz J, van Rossum G, Turco S. Effects of vanadyl sulfate on carbohydrate and lipid metabolism in patients with non—insulin-dependent diabetes mellitus. Metabolism. 1996;45(9):1130-1135. doi:10.1016/s0026-0495(96)90013-x.
- Goldfine A, Simonson D, Folli F, Patti M, Kahn C. Metabolic effects of sodium metavanadate in humans with insulin-dependent and noninsulin-dependent diabetes mellitus in vivo and in vitro studies. The Journal of Clinical Endocrinology & Metabolism. 1995;80(11):3311-3320. doi:10.1210/jcem.80.11.7593444.
- Cusi K, Cukier S, DeFronzo R, Torres M, Puchulu F, Redondo J. Vanadyl Sulfate Improves Hepatic and Muscle Insulin Sensitivity in Type 2 Diabetes1. The Journal of Clinical Endocrinology & Metabolism. 2001;86(3):1410-1417. doi:10.1210/jcem.86.3.7337.
- Vogler B, Ernst E. Aloe vera: a systematic review of its clinical effectiveness. Br J Gen Pract. 1999;49(447):823-828.
- Yongchaiyudha S, Rungpitarangsi V, Bunyapraphatsara N, Chokechaijaroenporn O. Antidiabetic activity of Aloe vera L. juice. I. Clinical trial in new cases of diabetes mellitus. Phytomedicine. 1996;3(3):241-243. doi:10.1016/s0944-7113(96)80060-2.
- Bunyapraphatsara N, Yongchaiyudha S, Rungpitarangsi V, Chokechaijaroenporn O. Antidiabetic activity of Aloe vera L. juice II. Clinical trial in diabetes mellitus patients in combination with glibenclamide. Phytomedicine. 1996;3(3):245-248. doi:10.1016/s0944-7113(96)80061-4.
- Huseini H, Kianbakht S, Hajiaghaee R, Dabaghian F. Anti-hyperglycemic and Anti-hypercholesterolemic Effects of aloe vera leaf Gel in Hyperlipidemic Type 2 Diabetic Patients: A Randomized Double-Blind Placebo-Controlled Clinical Trial. Planta Med. 2011;78(04):311-316. doi:10.1055/s-0031-1280474.
- Zhang Y, Liu W, Liu D, Zhao T, Tian H. Efficacy of Aloe Vera Supplementation on Prediabetes and Early Non-Treated Diabetic Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2016;8(7):388. doi:10.3390/nu8070388.
- Dick W, Fletcher E, Shah S. Reduction of Fasting Blood Glucose and Hemoglobin A1c Using Oral Aloe Vera: A Meta-Analysis. The Journal of Alternative and Complementary Medicine. 2016;22(6):450-457. doi:10.1089/acm.2015.0122.
- Suksomboon N, Poolsup N, Punthanitisarn S. Effect of aloe vera on glycaemic control in prediabetes and type 2 diabetes: a systematic review and meta-analysis. J Clin Pharm Ther. 2016;41(2):180-188. doi:10.1111/jcpt.12382.
- Vuksan V, Sievenpiper J, Koo V et al. American Ginseng (Panax quinquefolius L) Reduces Postprandial Glycemia in Nondiabetic Subjects and Subjects With Type 2 Diabetes Mellitus. Arch Intern Med. 2000;160(7):1009. doi:10.1001/archinte.160.7.1009.
- Vuksan V, Stavro M, Sievenpiper J et al. Similar postprandial glycemic reductions with escalation of dose and administration time of American ginseng in type 2 diabetes. Diabetes Care. 2000;23(9):1221-1226. doi:10.2337/diacare.23.9.1221.
- Sotaniemi E, Haapakoski E, Rautio A. Ginseng Therapy in Non-Insulin-Dependent Diabetic Patients: Effects on psychophysical performance, glucose homeostasis, serum lipids, serum aminoterminal propeptide concentration, and body weight. Diabetes Care. 1995;18(10):1373-1375. doi:10.2337/diacare.18.10.1373.
- Zhang Y, Li X, Zou D et al. Treatment of Type 2 Diabetes and Dyslipidemia with the Natural Plant Alkaloid Berberine. The Journal of Clinical Endocrinology & Metabolism. 2008;93(7):2559-2565. doi:10.1210/jc.2007-2404.
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717. doi:10.1016/j.metabol.2008.01.013.
- Zhang H, Wei J, Xue R et al. Berberine lowers blood glucose in type 2 diabetes mellitus patients through increasing insulin receptor expression. Metabolism. 2010;59(2):285-292. doi:10.1016/j.metabol.2009.07.029.
- Lan J, Zhao Y, Dong F et al. Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. J Ethnopharmacol. 2015;161:69-81. doi:10.1016/j.jep.2014.09.049.
- Bamosa A, Kaatabi H, Lebda F, Elq A, Al-Sultanb A. Effect of Nigella sativa seeds on the glycemic control of patients with type 2 diabetes mellitus. Indian J Physiol Pharmacol. 2010;54(4):44-354.
- Kaatabi H, Bamosa A, Badar A et al. Nigella sativa Improves Glycemic Control and Ameliorates Oxidative Stress in Patients with Type 2 Diabetes Mellitus: Placebo Controlled Participant Blinded Clinical Trial. PLoS ONE. 2015;10(2):e0113486. doi:10.1371/journal.pone.0113486.
- Badar A, Kaatabi H, Bamosa A et al. Effect of Nigella sativa supplementation over a one-year period on lipid levels, blood pressure and heart rate in type-2 diabetic patients receiving oral hypoglycemic agents: nonrandomized clinical trial. Ann Saudi Med. 2017;37(1):56-63. doi:10.5144/0256-4947.2017.56.
- Anderson J, Allgood L, Turner J, Oeltgen P, Daggy B. Effects of psyllium on glucose and serum lipid responses in men with type 2 diabetes and hypercholesterolemia. Am J Clin Nutr. 1999;70(4):466-473. doi:10.1093/ajcn/70.4.466.
- Pastors J, Blaisdell P, Balm T, Asplin C, Pohl S. Psyllium fiber reduces rise in postprandial glucose and insulin concentrations in patients with non-insulin-dependent diabetes. Am J Clin Nutr. 1991;53(6):1431-1435. doi:10.1093/ajcn/53.6.1431.
- Wolever T, Vuksan V, Eshuis H et al. Effect of method of administration of psyllium on glycemic response and carbohydrate digestibility. J Am Coll Nutr. 1991;10(4):364-371. doi:10.1080/07315724.1991.10718164.
- Frati Munari A, Benítez Pinto W, Raúl Ariza Andraca C, Casarrubias M. Lowering glycemic index of food by acarbose and Plantago psyllium mucilage. Arch Med Res. 1998;29(2):137-41.
- Rodrı́guez-Morán M, Guerrero-Romero F, Lazcano-Burciaga G. Lipid- and Glucose-Lowering Efficacy of Plantago Psyllium in Type II Diabetes. J Diabetes Complicat. 1998;12(5):273-278. doi:10.1016/s1056-8727(98)00003-8.
- Sierra M, García J, Fernández N, Diez M, Calle A. Therapeutic effects of psyllium in type 2 diabetic patients. Eur J Clin Nutr. 2002;56(9):830-842. doi:10.1038/sj.ejcn.1601398.
- Ziai S, Larijani B, Akhoondzadeh S et al. Psyllium decreased serum glucose and glycosylated hemoglobin significantly in diabetic outpatients. J Ethnopharmacol. 2005;102(2):202-207. doi:10.1016/j.jep.2005.06.042.
- Sartore G, Reitano R, Barison A et al. The effects of psyllium on lipoproteins in type II diabetic patients. Eur J Clin Nutr. 2009;63(10):1269-1271. doi:10.1038/ejcn.2009.60.
- Salazar-Martinez E, Willett W, Ascherio A et al. Coffee consumption and risk for type 2 diabetes mellitus. Ann Intern Med. 2004;140(1):1-8.
- Iso H, Date C, Wakai K, Fukui M, Tamakoshi A. The Relationship between Green Tea and Total Caffeine Intake and Risk for Self-Reported Type 2 Diabetes among Japanese Adults. Ann Intern Med. 2006;144(8):554. doi:10.7326/0003-4819-144-8-200604180-00005.
- van Dieren S, Uiterwaal C, van der Schouw Y et al. Coffee and tea consumption and risk of type 2 diabetes. Diabetologia. 2009;52(12):2561-2569. doi:10.1007/s00125-009-1516-3.
- Pimentel G, Zemdegs J, Theodoro J, Mota J. Does long-term coffee intake reduce type 2 diabetes mellitus risk?. Diabetol Metab Syndr. 2009;1(1):6. doi:10.1186/1758-5996-1-6
- Meyer K, Kushi L, Jacobs D, Slavin J, Sellers T, Folsom A. Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr. 2000;71(4):921-930. doi:10.1093/ajcn/71.4.921.
- Jiang X, Zhang D, Jiang W. Coffee and caffeine intake and incidence of type 2 diabetes mellitus: a meta-analysis of prospective studies. Eur J Nutr. 2013;53(1):25-38. doi:10.1007/s00394-013-0603-x
- Pan A, Demark-Wahnefried W, Ye X et al. Effects of a flaxseed-derived lignan supplement on C-reactive protein, IL-6 and retinol-binding protein 4 in type 2 diabetic patients. British Journal of Nutrition. 2008;101(08):1145. doi:10.1017/s0007114508061527.
- Pan A, Sun J, Chen Y et al. Effects of a Flaxseed-Derived Lignan Supplement in Type 2 Diabetic Patients: A Randomized, Double-Blind, Cross-Over Trial. PLoS ONE. 2007;2(11):e1148. doi:10.1371/journal.pone.0001148.
- Mani U, Mani I, Biswas M, Kumar S. An Open-Label Study on the Effect of Flax Seed Powder (Linum usitatissimum) Supplementation in the Management of Diabetes Mellitus. J Diet Suppl. 2011;8(3):257-265. doi:10.3109/19390211.2011.593615.
- Rhee Y, Brunt A. Flaxseed supplementation improved insulin resistance in obese glucose intolerant people: a randomized crossover design. Nutr J. 2011;10(1). doi:10.1186/1475-2891-10-44.
- Hutchins A, Brown B, Cunnane S, Domitrovich S, Adams E, Bobowiec C. Daily flaxseed consumption improves glycemic control in obese men and women with pre-diabetes: a randomized study. Nutrition Research. 2013;33(5):367-375. doi:10.1016/j.nutres.2013.02.012.
- Cairella M, Marchini G. Evaluation of the action of glucomannan on metabolic parameters and on the sensation of satiation in overweight and obese patients. Clin Ter. 1995;146(4):269-274.
- Chen H, Sheu W, Tai T, Liaw Y, Chen Y. Konjac Supplement Alleviated Hypercholesterolemia and Hyperglycemia in Type 2 Diabetic Subjects—A Randomized Double-Blind Trial. J Am Coll Nutr. 2003;22(1):36-42. doi:10.1080/07315724.2003.10719273.
- Vuksan V, Jenkins D, Spadafora P et al. Konjac-mannan (glucomannan) improves glycemia and other associated risk factors for coronary heart disease in type 2 diabetes. A randomized controlled metabolic trial. Diabetes Care. 1999;22(6):913-919. doi:10.2337/diacare.22.6.913.
- Chearskul S, Sangurai S, Nitiyanant W, Kriengsinyos W, Kooptiwut S, Harindhanavudhi T. Glycemic and lipid responses to glucomannan in Thais with type 2 diabetes mellitus. J Med Assoc Thai. 2007;90(10):2150-2157.
- Sood N, Baker W, Coleman C. Effect of glucomannan on plasma lipid and glucose concentrations, body weight, and blood pressure: systematic review and meta-analysis. Am J Clin Nutr. 2008;88(4):1167-1175. doi:10.1093/ajcn/88.4.1167.
- Huang, C. Y., Zhang, M. Y., Peng, S. S., Hong, J. R., Wang, X., Jiang, H. J., Zhang, F. L., Bai, Y. X., Liang, J. Z., Yu, Y. R. Effect of Konjac food on blood glucose level in patients with diabetes. Biomed.Environ.Sci 1990;3(2):123-131.
- Meyer K, Kushi L, Jacobs D, Slavin J, Sellers T, Folsom A. Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr. 2000;71(4):921-930. doi:10.1093/ajcn/71.4.921.
- Song Y, Manson J, Buring J, Liu S. Dietary Magnesium Intake in Relation to Plasma Insulin Levels and Risk of Type 2 Diabetes in Women. Diabetes Care. 2003;27(1):59-65. doi:10.2337/diacare.27.1.59.
- Fung T, Manson J, Solomon C, Liu S, Willett W, Hu F. The Association between Magnesium Intake and Fasting Insulin Concentration in Healthy Middle-Aged Women. J Am Coll Nutr. 2003;22(6):533-538. doi:10.1080/07315724.2003.10719332.
- Lopez-Ridaura R, Willett W, Rimm E et al. Magnesium Intake and Risk of Type 2 Diabetes in Men and Women. Diabetes Care. 2003;27(1):134-140. doi:10.2337/diacare.27.1.134.
- Huerta M, Roemmich J, Kington M et al. Magnesium Deficiency Is Associated With Insulin Resistance in Obese Children. Diabetes Care. 2005;28(5):1175-1181. doi:10.2337/diacare.28.5.1175.
- Schulze M, Schulz M, Heidemann C, Schienkiewitz A, Hoffmann K, Boeing H. Fiber and Magnesium Intake and Incidence of Type 2 Diabetes. Arch Intern Med. 2007;167(9):956-965. doi:10.1001/archinte.167.9.956.
- Cesarone MR, Incandela L, De Sanctis MT, et al. Evaluation of treatment of diabetic microangiopathy with total triterpenic fraction of Centella asiatica: a clinical prospective randomized trial with a microcirculatory model. Angiology 2001;52 Suppl 2:S49-54.
- Incandela L, Belcaro G, Cesarone MR, et al. Treatment of diabetic microangiopathy and edema with total triterpenic fraction of Centella asiatica: a prospective, placebo-controlled randomized study. Angiology 2001;52 Suppl 2:S27-31
- Leatherdale B, Panesar R, Singh G, Atkins T, Bailey C, Bignell A. Improvement in glucose tolerance due to Momordica charantia (karela). BMJ. 1981;282(6279):1823-1824. doi:10.1136/bmj.282.6279.1823.
- Welihinda J, Karunanayake E, Sheriff M, Jayasinghe K. Effect of Momordica charantia on the glucose tolerance in maturity onset diabetes. J Ethnopharmacol. 1986;17(3):277-282. doi:10.1016/0378-8741(86)90116-9.
- Srivastava Y, Venkatakrishna-Bhatt H, Verma Y, Venkaiah K, Raval B. Antidiabetic and adaptogenic properties ofMomordica charantia extract: An experimental and clinical evaluation. Phytotherapy Research. 1993;7(4):285-289. doi:10.1002/ptr.2650070405.
- Baldwa V, Bhandari C, Pangaria A, Goyal R. Clinical Trial in Patients with Diabetes Mellitus of an Insulin-like Compound Obtained from Plant Source. Ups J Med Sci. 1977;82(1):39-41. doi:10.3109/03009737709179057.
- Rahman I, Khan R, Rahman K, Bashir M. Lower hypoglycemic but higher antiatherogenic effects of bitter melon than glibenclamide in type 2 diabetic patients. Nutr J. 2015;14(1). doi:10.1186/1475-2891-14-13.
- Ahmad N, Hassan MR, Halder H, Bennoor KS. Effect of Momordica charantia (Karolla) extracts on fasting and postprandial serum glucose levels in NIDDM patients (abstract). Bangladesh Med Res Counc Bull 1999;25:11-3.
- Dresden, Danielle. Effects of Diabetes On the Body and Organs. Medical News Today. https://www.medicalnewstoday.com/articles/317483.php. Accessed June 11, 2019.
- Fletcher, Jenna. Diabetic What To Know About Diabetic Gastroparesis. Medical News Today. https://www.medicalnewstoday.com/articles/324964.php. Accessed June 11, 2019.
- What Is a Silent Heart Attack? Go Red for Women. https://www.goredforwomen.org/en/about-heart-disease-in-women/facts/silent-heart-attack-symptoms-risks. Accessed June 11, 2019.
- The Danger of “Silent” Heart Attacks. Harvard Health Publishing. https://www.health.harvard.edu/heart-health/the-danger-of-silent-heart-attacks.
- Torbati, Masoud, Meshkini, Ali, Abri-Aghdam, Babak, Amir Farhangi, Saba. Assessing the correlation of trauma severity, blood sugar level, and neurologic outcomes in traumatic spinal cord injury patients. JARCM. https://jarcm.tbzmed.ac.ir/PDF/JARCM_2526_20141211135605. Accessed June 11, 2019
- Diabetes Prevalence. Diabetes.co.uk: the global diabetes community. https://www.diabetes.co.uk/diabetes-prevalence.html. Accessed June 11, 2019.
- Semeco, Arlene, MS, RD. 15 Ways to Lower Blood Sugar Levels Naturally. Healthline. https://www.healthline.com/nutrition/15-ways-to-lower-blood-sugar#section9. Accessed June 11, 2019.