WHAT IS BLOOD PRESSURE?
Blood pressure is the force of blood flow within the blood vessels of the body. There are two types of blood pressure; diastolic pressure, which is the measured pressure when the heart is resting as it fills with blood; and systolic pressure, which is the measured pressure during contractions of the heart as it pushes blood out to the arteries. The importance of maintaining a healthy blood pressure is significant as blood pressure can affect the entire body. With a healthy blood pressure, organs in the body receive the appropriate volumes of blood required to function optimally (1).
Blood pressure is measured in millimeters of mercury (mm Hg) and recorded as systolic pressure over diastolic pressure. An example of a health measurement of blood pressure is 120/80 mm Hg (2,3).
Blood pressure can fluctuate depending on the activity a person is engaging in; for example, blood pressure is lower when a person is sleeping but elevated when running. These fluctuations are considered normal, as the blood pressure usually returns to a normal level (4,5).
With abnormal blood pressure, there could be too much blood flow, resulting in prolonged high blood pressure (hypertension) or too little blood flow, resulting in prolonged low blood pressure (hypotension). These conditions can lead to serious health problems, including mental deficits, renal failure, cardiovascular problems such as stroke or heart attacks and even comas. High blood pressure is categorized into stages based on increasing increments of measurements (1,5).
- Prehypertension is consistent blood pressure measurements between 120/80 and 139/89. A person who is prehypertensive has higher than normal blood pressure, which develops into hypertension if it is not treated or controlled.
- Stage 1 hypertension is consistent blood pressure measurements between 140/90 and 159/99.
- Stage 2 hypertension is consistent blood pressure measurements at or higher than 160/100 (4,5).
It is noteworthy that persons who have underlying conditions such as diabetes or chronic kidney disease will be diagnosed with high blood pressure at measurements of 130/80 mm Hg. Additionally, more attention is paid to the systolic number; therefore, if the systolic number is higher than normal, but the diastolic number is within a normal range, the person will be considered as having high blood pressure (5).
RISK FACTORS AND SYMPTOMS OF HYPERTENSION
Typically, there are no telling symptoms of hypertension. Possible clinical presentations may be headaches, nosebleeds or transient stroke (6).
There are numerous risk factors for hypertension. These can be considered lifestyle, medical, genetic or psychosocial factors.
Genetic Factors
While the exact genetic mechanism is not clearly understood, research has shown that persons who have one or both parents with hypertension are twice as likely to develop hypertension themselves. Estimates show that almost 50% of people who have high blood pressure have contributing genetic factors (7,8,9). Research has also shown that African Americans are at higher risk for developing hypertension compared to Caucasian Americans (10).
Medical Factors
Hypertension can be caused or exasperated due to a coexisting condition; in such cases, high blood pressure is known as secondary hypertension. Some of these diseases or conditions include diabetes, renal disease, neurological disorders, thyroid diseases, and pregnancy (11,12,13,14,15).
Additionally, certain medications and drugs can also lead to secondary hypertension. These include decongestants, steroids such as prednisone, estrogen (oral contraceptives), nonsteroidal anti-inflammatory medications (ibuprofen), psychiatric medications (Prozac), some herbal medications (ginseng) and illicit drugs (cocaine, amphetamines) (16).
Psychosocial Factors
Certain psychological and social aspects are also considered risk factors for hypertension. Research indicates that occupational stress, for example, long work hours, job control, security concerns, wages, and quality of jobs, are significantly associated with the development of hypertension (17,18). Mental health concerns are also associated with the risk of developing hypertension. Factors such as traumatic events, depression, and anxiety have all been associated with a higher prevalence of hypertension (19,20,21). Social integration and loneliness in middle-aged to older adults have also been associated with the risk of hypertension (22,23).
Lifestyle Factors
Certain lifestyle choices are risk factors for developing hypertension. One of the main risk factors for hypertension is obesity; research shows that poor nutrition and diet and lack of exercise leading to obesity can result in hypertension (24,25,26). Additionally, cigarette smoking and excessive alcohol consumption have also been associated with the risk of developing hypertension (24,27,28).
For more information on hypertension and diagnosis: 1. Talk to your doctor 2. Visit the Mayo Clinic website 3. Visit the American Heart Association website 4. Visit the Centers for Disease Control and Prevention website
HYPERTENSION FACTS AND STATISTICS
Statistics for 2016 report that approximately 75 million adults in the United States (32% of the population) have high blood pressure. Estimates show that 1 in every 3 adults in the United States is prehypertensive. Nearly 50% of the 75 million adults with hypertension are either unaware of their condition, not getting any treatment at all, or treatment that is not helping (29,30).
Reports also indicate that one of the leading causes of death in the United States is high blood pressure, responsible for over 400,000 deaths in 2014 (29). Reports from 2015 show that 7 out of 10 adults who experienced their first heart attack had hypertension, and 8 out of 10 adults who experience their first stroke had hypertension (31).
MEDICAL TREATMENT OF HYPERTENSION
First line pharmacological treatment for hypertension include:
- Diuretics: Remove excess water from the body. Side-effects include dizziness, weakness, hypotension, muscle cramps, frequent urination, sensitivity to the sun, reduced potassium and calcium levels in the blood, elevated blood glucose, elevated uric acid in the urine (32,33).
- Angiotensin-converting enzyme (ACE) inhibitors: Work by inhibiting enzymes that make angiotensin, which is responsible for increasing blood pressure. Side effects include a dry cough, skin rash, headache, loss of taste sensitivity, nausea, and diarrhea (32,33).
- Angiotensin receptor blockers (ARBs): Inhibit the effect of angiotensin. Side-effects include fatigue, dizziness, headaches, low blood pressure, diarrhea and elevated blood potassium levels (32,33).
- Beta-blockers: Work by slowing down the pulse and reducing stress hormones effects on the heart. Side-effects include shortness of breath, fatigue, insomnia, dizziness, heart failure, impotence, high levels of triglycerides in the blood, mood changes and poor circulation (32,33).
- Calcium channel blockers: Work by expanding the blood vessels so the blood can flow easily. Side-effects include edema in the extremities, skin rash, fast heart rate, flushed face, nausea, fatigue, headache and dizziness (32,33).
- Vasodilators: Work by relaxing the smooth cells of the blood vessels for the blood to flow easily. Side-effects include rapid heart rate, headache, nausea and diarrhea, and excessive hair growth (32).
NATURAL WAYS TO HELP SUPPORT HEALTHY BLOOD PRESSURE
Practices to Help Support Healthy Blood Pressure:
- Healthy diets: high in fruits and vegetables but low in salt, dairy, and fat
- Increase physical activity
- Stop smoking
- Reduce alcohol consumption (34,35)
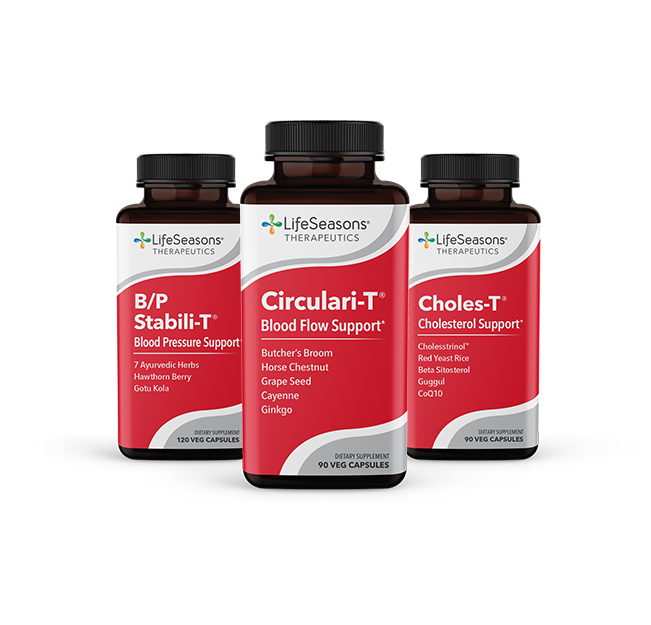
Natural Supplements That Help Support Healthy Blood Pressure:
- Hawthorn Berry (38,39)
- Ashwagandha (37,40)
REFERENCES
- Brzezinski W. Blood Pressure. Clinical Methods: The History, Physical, And Laboratory Examinations. 3rd ed. https://www.ncbi.nlm.nih.gov/books/NBK268/. Accessed April 10, 2018.
- Blood Pressure – PubMed Health. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0023514/. Accessed April 10, 2018.
- Understanding Blood Pressure Readings. http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/KnowYourNumbers/Understanding-Blood-Pressure-Readings_UCM_301764_Article.jsp?appName=WebApp#.WsuPwi7wa70. Accessed April 10, 2018.
- Measuring Your Blood Pressure at Home. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0041082/#conssmbp.s3. Accessed April 10, 2018.
- High Blood Pressure. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0062996/. Accessed April 11, 2018.
- Ashley E, Niebauer J. Hypertension. https://www.ncbi.nlm.nih.gov/books/NBK2217/. Accessed April 11, 2018.
- Beevers G, Lip G, O’Brien E. The pathophysiology of hypertension. BMJ. 2001;322(7291):912-916. doi:10.1136/bmj.322.7291.912.
- Butler M. PEDIATRIC HYPERTENSION GENETICS OF HYPERTENSION • CURRENT STATUS. The Lebanese Medical Journal. 2010;58(3):175-178.
- Franceschini N, Chasman DI, Cooper-DeHoff RM, Arnett DK. Genetics, Ancestry, and Hypertension: Implications for Targeted Antihypertensive Therapies. Curr Hypertens Rep. 2014;16(8). doi:10.1007/s11906-014-0461-9.
- Lackland D. Racial Differences in Hypertension: Implications for High Blood Pressure Management. Am J Med Sci. 2014;348(2):135-138. doi:10.1097/maj.0000000000000308.
- Long A, Dagogo-Jack S. Comorbidities of Diabetes and Hypertension: Mechanisms and Approach to Target Organ Protection. The Journal of Clinical Hypertension. 2011;13(4):244-251. doi:10.1111/j.1751-7176.2011.00434.x.
- Noh J, Kim H, Shin A et al. Prevalence of Comorbidity among People with Hypertension: The Korea National Health and Nutrition Examination Survey 2007-2013. Korean Circ J. 2016;46(5):672. doi:10.4070/kcj.2016.46.5.672.
- Faselis C, Doumas M, Papademetriou V. Common Secondary Causes of Resistant Hypertension and Rational for Treatment. Int J Hypertens. 2011;2011:1-17. doi:10.4061/2011/236239.
- Kattah AG, Garovic VD. The Management of Hypertension in Pregnancy. Adv Chronic Kidney Dis. 2013;20(3):229-239. doi:10.1053/j.ackd.2013.01.014.
- Aronow WS. Hypertensive disorders in pregnancy. Ann Transl Med. 2017;5(12):266-266. doi:10.21037/atm.2017.03.104.
- Viera A, Neutze D. Diagnosis of Secondary Hypertension: An Age-Based Approach. Am Fam Physician. 2010;82(12):1471-1478.
- Modrek S, Cullen M. Health consequences of the ‘Great Recession’ on the employed: Evidence from an industrial cohort in aluminum manufacturing. Social Science & Medicine. 2013;92:105-113. doi:10.1016/j.socscimed.2013.04.027.
- Smith P, Mustard C, Lu H, Glazier R. Comparing the risk associated with psychosocial work conditions and health behaviours on incident hypertension over a nine-year period in Ontario, Canada. Canadian Journal of Public Health. 2013;104(1):82-86.
- Chaudieu I, Norton J, Ritchie K, Birmes P, Vaiva G, Ancelin M. Late-Life Health Consequences of Exposure to Trauma in a General Elderly Population. J Clin Psychiatry. 2011;72(07):929-935. doi:10.4088/jcp.10m06230.
- Ginty AT, Carroll D, Roseboom TJ, Phillips AC, de Rooij SR. Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. J Hum Hypertens. 2012;27(3):187-190. doi:10.1038/jhh.2012.18.
- Nabi H, Chastang J, Lefevre T et al. Trajectories of Depressive Episodes and Hypertension Over 24 Years: The Whitehall II Prospective Cohort Study. Hypertension. 2011;57(4):710-716. doi:10.1161/hypertensionaha.110.164061.
- Hawkley L, Thisted R, Masi C, Cacioppo J. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132-141. doi:10.1037/a0017805.
- Yang YC, et al. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health. 2013;13(1). doi:10.1186/1471-2458-13-1210.
- Ibekwe R. Modifiable risk factors of hypertension and socio-demographic profile in Oghara, Delta State; prevalence and correlates. Annals of Medical and Health Sciences Research. 2015;5(1):71. doi:10.4103/2141-9248.149793.
- Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp Ther Med. 2016;12(4):2395-2399. doi:10.3892/etm.2016.3667.
- Aronow W. Association of obesity with hypertension. Ann Transl Med. 2017;5(17):350-350. doi:10.21037/atm.2017.06.69.
- Husain K, Ansari R, Ferder L. Alcohol-induced hypertension: Mechanism and prevention. World J Cardiol. 2014;6(5):245. doi:10.4330/wjc.v6.i5.245.
- Gao K, Shi X, Wang W. The life-course impact of smoking on hypertension, myocardial infarction and respiratory diseases. Sci Rep. 2017;7(1). doi:10.1038/s41598-017-04552-5.
- High Blood Pressure Fact Sheet|Data & Statistics|DHDSP|CDC. https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm. Accessed April 12, 2018.
- Merai R, Siegel C, Rakotz M et al. CDC Grand Rounds: A Public Health Approach to Detect and Control Hypertension. MMWR Morb Mortal Wkly Rep. 2016;65(45):1261-1264. doi:10.15585/mmwr.mm6545a3.
- High Blood Pressure (Hypertension) Information https://www.cdc.gov/bloodpressure/index.htm. Accessed April 12, 2018.
- Nguyen Q, Dominguez J, Nguyen L, Gullapalli N. Hypertension Management: An Update. American Health and Drug Benefits. 2010;3(1):47-56.
- What medications are used to treat high blood pressure? https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072414/. Accessed April 12, 2018.
- Collier S, Landram MJ. Treatment of prehypertension: lifestyle and/or medication. Vasc Health Risk Manag. 2012:613. doi:10.2147/vhrm.s29138.
- Nicoll R, Henein M. Hypertension and lifestyle modification: how useful are the guidelines?. British Journal of General Practice. 2010;60(581):879-880. doi:10.3399/bjgp10x544014.
- Dwivedi S, Chopra D. Revisiting Terminalia arjuna – An Ancient Cardiovascular Drug. J Tradit Complement Med. 2014;4(4):224-231. doi:10.4103/2225-4110.139103.
- Sandhu J, Shah B, Shenoy S, Padhi M, Chauhan S, Lavekar G. Effects of Withania somnifera (Ashwagandha) and Terminalia arjuna (Arjuna) on physical performance and cardiorespiratory endurance in healthy young adults. International Journal of Ayurveda Research. 2010;1(3):144. doi:10.4103/0974-7788.72485.
- Walker A, Marakis G, Morris A, Robinson P. Promising hypotensive effect of hawthorn extract: A randomized double-blind pilot study of mild, essential hypertension. Phytotherapy Research. 2002;16(1):48-54. doi:10.1002/ptr.947.
- Dahmer S, Scott E. Health Effects of Hawthorn. Am Fam Physician. 2010;81(4):465-468.
- Singh N, Bhalla M, De Jager P, Gilca M. An Overview on Ashwagandha: A Rasayana (Rejuvenator) of Ayurveda. African Journal of Traditional, Complementary and Alternative Medicines. 2011;8(5S). doi:10.4314/ajtcam.v8i5s.9.