WHAT ARE MIGRAINES?
Migraines are a common disorder of painful, debilitating pain localized to one side of the head. They have been known to last up to 72 hours (1). Some warning signs before a migraine begins are flashes of light, blind spots, or a tingling on one side of the body. With large amounts of data that links migraines to trigger factors, it is clear that migraines require activation of meningeal nociceptors to exert a powerful effect on the sensory neurons (2,3).
Furthermore, according to the World Health Organization, migraines are one of the most globally prevalent reasons for medical care (4). It has been reported that the number of cases of migraines are higher in women than in men around the world (4). Overall, there are many studies that have analyzed the way that migraines have affected the quality of people’s lives as well as the disabilities migraine patients may have (5).
RISK FACTORS OF MIGRAINES
- Stress: There is a complex relationship between migraines and stress. Studies have shown that 50% to 80% of patients who report stress symptoms have also reported migraines attacks (6,7).
- Changes in levels of hormones: Migraine attacks are more prevalent in women than in men. Furthermore, natural changes that occur in women such as changes in endogenous sex hormones and exogenous sex hormones, are also known to trigger migraine attacks (8).
- Dietary products: A range of 12% to 60% of patients who have reported a migraine that was triggered by a specific food or combination of foods. Dietary products such as chocolate, cheese, and alcohol are the top three that were found to be triggers of migraine attacks (9).
- Environmental changes: Migraines are also known to be caused by environmental triggers such as bright sunlight or flickering of lights. Furthermore, patients who have suffered a migraine attack, also describe air quality and odors as triggers for a migraine (10).
- Genetic Factors: Family and twin studies have shown that there is a genetic linking to migraines, but studies have not been able to identify which gene is predisposing to the development of the disease (11,12).
SYMPTOMS OF MIGRAINES
- Nausea: Experienced by one-third of the patients who are experiencing or have experienced migraines (13)
- Vomiting (14)
- Hypersensitivity to light and sound (15,16)
For more information on migraines and diagnosis: 1. Talk to your doctor 2. Visit the Migraine Research Foundation website 3. Visit the Mayo Clinic website 4. Visit the American Migraine Foundation website
FACTS AND STATISTICS ON MIGRAINES
According to the 2012 Global Burden of Disease study, migraine is the 8th most burdensome disease in the world (17). In 2012, data reports showed that 14.2% of adults in the United States who were 18 years or older reported having a migraine (18). Research shows that migraines affect females up to 3 times more than males (19,20).
In 2015, 20.0% of women and 9.7% of men, 18 years and older reported a severe headache or migraine within 3 months of the survey. For both sexes, reports of severe headaches or migraines decreased with increased age. Of men in the age groups 18 to 44 years old, 11% reported a severe headache or migraine, while only 3.4% reported severe headaches or migraines in the group over 75 years old. Of women in the age groups 18 to 44 years old, 24.7% reported a severe headache or migraine, while only 6.3% reported severe headaches or migraines in the group over 75 years old (21).
MEDICAL TREATMENT OF MIGRAINES
Preventative treatments and drugs can only be used on patients where there is a known headache trigger (22).
- Tricyclic antidepressants: This anti-depressant is one of the most common ones used for migraine prevention. Furthermore, it is also the only known anti-depressant that has been fully proven to work towards the prevention of future migraine attacks (22). Common side effects include blurred vision, dry mouth, constipation, weight gain or loss, low blood pressure on standing, rash, hives, and increased heart rate (23).
- Antiepileptic drugs: This type of drug is known for its mechanism of inhibiting or blocking gated sodium channels in neural processes (24).
- Gabapentin (22)
- Valproic Acid (25)
- Lamotrigine (26)
- Angiotensin (27)
- Histamines (28,29)
NATURAL WAYS TO HELP ALLEVIATE HEAD PAIN
Practices to Help Alleviate Head Pain:
- Changes in lifestyle to help to reduce triggers like food triggers (30)
- Proper management of headaches, depression, anxiety, pain syndromes and other conditions (30)
- Stress management (31)
Natural Supplements That Help Alleviate Head Pain:
- Feverfew Leaf (32,33)
- Butterbur (34,35)
- White Willow Bark (36)
- Magnesium Citrate (37,38)
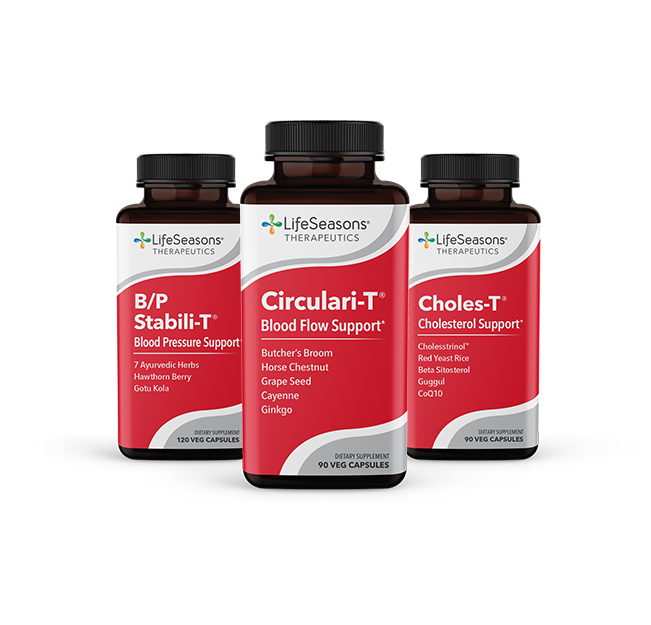
- CoQ10 (39,40)
REFERENCES
- The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808. doi:10.1177/0333102413485658.
- Levy D, Strassman A, Burstein R. A Critical View on the Role of Migraine Triggers in the Genesis of Migraine Pain. Headache: The Journal of Head and Face Pain. 2009;49(6):953-957. doi:10.1111/j.1526-4610.2009.01444.x.
- Strassman A, Raymond S, Burstein R. Sensitization of meningeal sensory neurons and the origin of headaches. Nature. 1996;384(6609):560-564. doi:10.1038/384560a0.
- Shaik M, Hassan N, Tan H, Gan S. Quality of Life and Migraine Disability among Female Migraine Patients in a Tertiary Hospital in Malaysia. Biomed Res Int. 2015; 2015:1-9. doi:10.1155/2015/523717.
- Tulen J, Stronks D, Bussmann J, Pepplinkhuizen L, Passchier J. Towards an objective quantitative assessment of daily functioning in migraine: a feasibility study. Pain. 2000;86(1):139-149. doi:10.1016/s0304-3959(00)00235-9.
- Radat F. Stress et migraine. Rev Neurol (Paris). 2013;169(5):406-412. doi:10.1016/j.neurol.2012.11.008.
- Peroutka S. What Turns on a Migraine? A Systematic Review of Migraine Precipitating Factors. Curr Pain Headache Rep. 2014;18(10). doi:10.1007/s11916-014-0454-z.
- Chai N, Peterlin B, Calhoun A. Migraine and estrogen. Curr Opin Neurol. 2014;27(3):315-324. doi:10.1097/wco.0000000000000091.
- Finocchi C, Sivori G. Food as trigger and aggravating factor of migraine. Neurological Sciences. 2012;33(S1):77-80. doi:10.1007/s10072-012-1046-5.
- Friedman D, De Ver Dye T. Migraine and the Environment. Headache: The Journal of Head and Face Pain. 2009;49(6):941-952. doi:10.1111/j.1526-4610.2009.01443.x.
- Piane M, Lulli P, Farinelli I et al. Genetics of migraine and pharmacogenomics: some considerations. J Headache Pain. 2007;8(6):334-339. doi:10.1007/s10194-007-0427-2.
- Gasparini C, Sutherland H, Griffiths L. Studies on the Pathophysiology and Genetic Basis of Migraine. Curr Genomics. 2013;14(5):300-315. doi:10.2174/13892029113149990007.
- Maniyar F, Sprenger T, Schankin C, Goadsby P. The origin of nausea in migraine–A PET study. J Headache Pain. 2014;15(1). doi:10.1186/1129-2377-15-84.
- Gasparini C, Smith R, Griffiths L. Genetic and biochemical changes of the serotonergic system in migraine pathobiology. J Headache Pain. 2017;18(1). doi:10.1186/s10194-016-0711-0.
- Luzeiro I, Luís L, Gonçalves F, Pavão Martins I. Vestibular Migraine: Clinical Challenges and Opportunities for Multidisciplinarity. Behav Neurol. 2016;2016:1-11. doi:10.1155/2016/6179805.
- Evans R, Seifert T, Kailasam J, Mathew N. The Use of Questions to Determine the Presence of Photophobia and Phonophobia During Migraine. Headache: The Journal of Head and Face Pain. 2007;48(3):395-397. doi:10.1111/j.1526-4610.2007.00920.x.
- Vos T, Flaxman A, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2163-2196. doi:10.1016/s0140-6736(12)61729-2.
- Burch R, Loder S, Loder E, Smitherman T. The Prevalence and Burden of Migraine and Severe Headache in the United States: Updated Statistics From Government Health Surveillance Studies. Headache: The Journal of Head and Face Pain. 2015;55(1):21-34. doi:10.1111/head.12482.
- Lay C, Broner S. Migraine in Women. Neurol Clin. 2009;27(2):503-511. doi:10.1016/j.ncl.2009.01.002.
- Sacco S, Ricci S, Degan D, Carolei A. Migraine in women: the role of hormones and their impact on vascular diseases. J Headache Pain. 2012;13(3):177-189. doi:10.1007/s10194-012-0424-y.
- QuickStats: Percentage* of Adults Aged ≥18 Years Who Reported Having a Severe Headache or Migraine in the Past 3 Months,† by Sex and Age Group — National Health Interview Survey,§ United States, 2015. 2018. https://www.cdc.gov/mmwr/volumes/66/wr/mm6624a8.htm
- Silberstein S. Preventive Migraine Treatment. CONTINUUM: Lifelong Learning in Neurology. 2015;21:973-989. doi:10.1212/con.0000000000000199.
- TRICYCLIC ANTIDEPRESSANTS (TCAS). https://www.rxlist.com/tricyclic_antidepressants_tcas/drugs-condition.htm. Accessed June 25, 2018.
- Bromfield E, Cavazos J, Sirven J. Neuropharmacology of Antiepileptic Drugs. Ncbinlmnihgov. 2018. https://www.ncbi.nlm.nih.gov/books/NBK2513/. Accessed March 19, 2018.
- Valproic acid Uses, Side Effects & Warnings – Drugs.com. 2018. https://www.drugs.com/mtm/valproic-acid.html. Accessed March 19, 2018.
- Lamotrigine Uses, Side Effects & Warnings – Drugs.com. 2018. Available at: https://www.drugs.com/mtm/lamotrigine.html. Accessed March 19, 2018.
- Parveen S, Javed M. Stevens Johnson Syndrome associated with Lamotrigine. Pak J Med Sci. 2013;29(6). doi:10.12669/pjms.296.4385.
- Millán-Guerrero R, Isais-Millán R, Benjamín T, Tene C. Nα -Methyl Histamine Safety and Efficacy in Migraine Prophylaxis: Phase III Study. Canadian Journal of Neurological Sciences / Journal Canadien des Sciences Neurologiques. 2006;33(02):195-199. doi:10.1017/s0317167100004960.
- Millán-Guerrero R, Isais-Millán R, Barreto-Vizcaíno S et al. Subcutaneous Histamine versus Topiramate in Migraine Prophylaxis: A Double-Blind Study. Eur Neurol. 2008;59(5):237-242. doi:10.1159/000115637.
- Weatherall M. The diagnosis and treatment of chronic migraine. Ther Adv Chronic Dis. 2015;6(3):115-123. doi:10.1177/2040622315579627.
- Weatherby S, Brown H, Newman C, Noad R. Behavioural management of migraine. Ann Indian Acad Neurol. 2012;15(5):78. doi:10.4103/0972-2327.100018.
- Pareek A, Suthar M, Rathore G, Bansal V. Feverfew (Tanacetum parthenium L.): A systematic review. Pharmacogn Rev. 2011;5(9):103. doi:10.4103/0973-7847.79105.
- Pfaffenrath V, Diener H, Fischer M, Friede M, Henneicke-von Zepelin H. The Efficacy and Safety of Tanacetum Parthenium (Feverfew) in Migraine Prophylaxis—a Double-Blind, Multicentre, Randomized Placebo-Controlled Dose-Response Study. Cephalalgia. 2002;22(7):523-532. doi:10.1046/j.1468-2982.2002.00396.x.
- Benemei S, De Logu F, Li Puma S et al. The anti-migraine component of butterbur extracts, isopetasin, desensitizes peptidergic nociceptors by acting on TRPA1 cation channel. Br J Pharmacol. 2017;174(17):2897-2911. doi:10.1111/bph.13917.
- Lipton R, Gobel H, Einhaupl K, Wilks K, Mauskop A. Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology. 2004;63(12):2240-2244. doi:10.1212/01.wnl.0000147290.68260.11.
- Vlachojannis J, Cameron M, Chrubasik S. A systematic review on the effectiveness of willow bark for musculoskeletal pain. Phytotherapy Research. 2009;23(7):897-900. doi:10.1002/ptr.2747.
- von Luckner A, Riederer F. Magnesium in Migraine Prophylaxis-Is There an Evidence-Based Rationale? A Systematic Review. Headache: The Journal of Head and Face Pain. 2017;58(2):199-209. doi:10.1111/head.13217.
- Koseoglu E, Talaslioglu A, Gonul A, Kula M. The effects of magnesium prophylaxis in migraine without aura. Magnes Res. 2008;21(2):101-108.
- Gaul C, Diener H, Danesch U. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. J Headache Pain. 2015;16(1). doi:10.1186/s10194-015-0516-6.
- Sandor P, Di Clemente L, Coppola G et al. Efficacy of coenzyme Q10 in migraine prophylaxis: A randomized controlled trial. Neurology. 2005;64(4):713-715. doi:10.1212/01.wnl.0000151975.03598.ed.